RNFA Scope of Practice, Standards of Practice, and Certification
When considering your role and the tasks and duties you perform as a registered nurse first assistant (RNFA), there are three areas you must understand. These are your scope of practice, standards of practice, and certification.
Scope of Practice
The RNFA scope of practice is determined by your state board of nursing and the facility where you are employed. According to the American Nurses Association (n.d.), “Scope of practice describes the services that a qualified health professional is deemed competent to perform and permitted to undertake—in keeping with the terms of their professional license” (para 1).
All licensed health care professionals must practice within the scope or boundaries of their license. These boundaries are determined by the regulatory agency that oversees the license. In some states, there is no legislation regarding the RNFA scope of practice (AORN, 2022). In this case, the RNFA’s scope of practice is essentially determined by the facility where they are employed.
The AORN Position Statement on RN First Assistants (2018), has a section titled, Scope of Practice (p. 1) that states,
Registered nurse first assistant responsibilities in the perioperative arena include, but are not limited to,
- preoperative patient management in collaboration with other health care providers, such as
- performing focused preoperative nursing assessments and
- communicating and collaborating with other health care providers regarding the patient’s plan of care; and
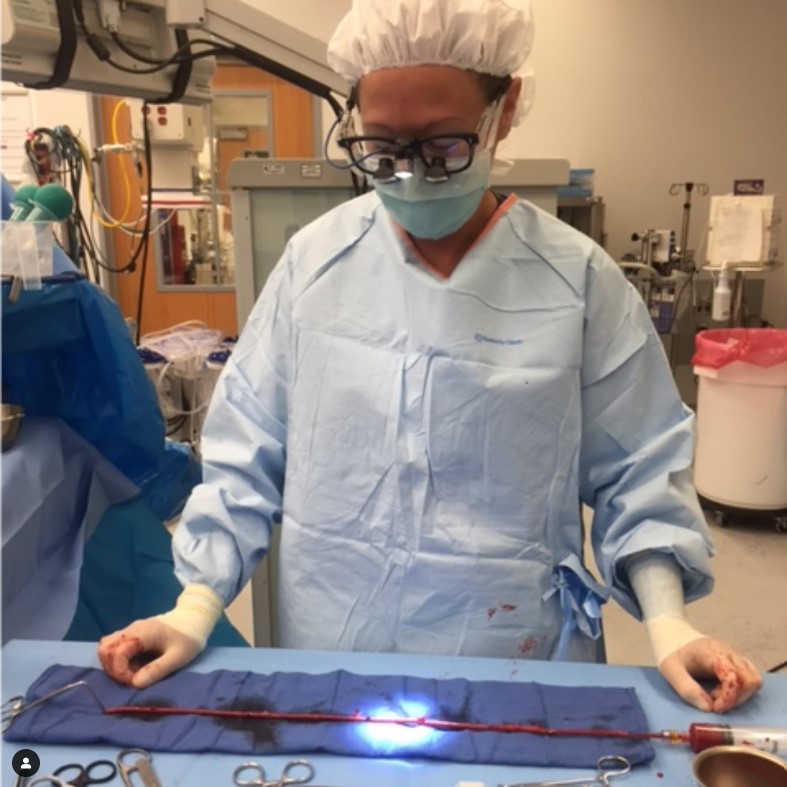
- intraoperative performance of surgical first assistant techniques, such as
- using instruments and medical devices,
- providing surgical site exposure,
- handling and/or cutting tissue,
- providing hemostasis,
- suturing, and
- wound management; and
- postoperative patient management in collaboration with other health care providers in the immediate postoperative period and beyond, such as
- participating in postoperative rounds and
- assisting with patient discharge planning and identifying appropriate community resources as needed.
Notably, the AORN is a professional organization, not a regulatory agency overseeing licensure; therefore, the AORN does not determine scope of practice for an RNFA. However, as experts in perioperative nursing, the AORN may discuss the duties and tasks performed by nurses assuming the RNFA role.
Standards of Practice
Standards of practice describe the level of care or performance common to the nursing specialty as recommended by experts in the specialty. Standards are often used to determine the quality of specialty nursing practice. The AORN makes recommendations and provides guidance for the RNFA in the AORN RNFA Standards of Practice (2013). The Standards were derived from previous versions of the RNFA Competency Statements and the Role-Specific Performance Evaluation Tool for the RNFA. As stated in the document (p. 1),
The standards delineate the responsibilities of the RNFA as he/she practices within the perioperative setting. As RNFAs progress from novice to expert, some will become more proficient than others at the various activities addressed in the standards. Not all RNFAs will practice all facets of the role at any given time; some RNFAs may never practice some facets of the role because their practice is limited by regulatory boundaries or facility policies. The standards focus on the specific responsibilities of the RNFA while remaining broad enough to allow for flexibility when applied to various practice settings.
Standard 5: Implementation of the AORN RNFA Standards of Practice (2013, pp. 3-7) provides a list of duties and tasks that may be performed by an RNFA.
Certification
Certification is the formal process by which a certifying agency validates a nurse’s knowledge, skills and abilities in a defined role and clinical area of practice, based on predetermined standards. The goal of certification is to create a culture of patient safety and extraordinary care. When a nurse achieves certification, it helps create this culture and it benefits the entire healthcare community−−from the patient to the nurse to the employer or hospital administrator. Becoming certified also demonstrates the nurse’s commitment to their own professional development. According to the American Association of Critical Care Nurses (n.d.), achieving board certification demonstrates to patients, employers, and the public that a nurse’s knowledge reflects national standards and a deep commitment to patient safety.
There is evidence to show that obtaining certification in a nursing specialty:
- promotes optimal patient outcomes,
- enhances the quality of care provided,
- provides a benchmark for verifying the competence of the provider,
- enhances patient safety by validating that nursing practice is consistent with the standards and recommendations of the professional nursing specialty organization,
- promotes continuing education and supports advanced education, and
- fosters personal growth, career advancement, and professional prestige (Stuckey & Wymer, 2020).
Achieving certification is supported by most professional societies, including the AORN. In 2019, the National Assistant at Surgery Certification (NASC; nascertification.com) became the official certifying organization for the CRNFA and RNAS-C credentials.
The RNAS-C and CRNFA are two levels of RNFA certification offered by the NASC.
- RNAS-C is for the novice RNFA with a minimum of 120 hours of practice in the RNFA role. A bachelor’s degree is not required. Certification is earned by passing a 150-question exam.
- CRNFA certification is for the experienced RNFA with a minimum of 2,000 hours of practice in the RNFA role who holds a bachelor’s degree or higher. Certification is earned by satisfactorily completing the CRNFA Professional Portfolio.
Neither the AORN nor the NASC distinguish between the tasks that may be performed by an RNFA, RNAS-C, or CRNFA. The AORN RNFA Standards of Practice (2013) do not vary based on certification.
According to the AORN Position Statement on RN First Assistants (2018, p.1)
Perioperative nursing is a specialized area of practice. Registered nurses practicing as first assistants in surgery are functioning in an expanded perioperative nursing role. First assisting responsibilities are further refinements of perioperative nursing practice and are executed within the context of the nursing process. These responsibilities include certain delegated medical functions that can be assumed by the RN who is qualified to practice as an RNFA. Registered nurse first assistant responsibilities may vary depending on patient populations, practice environments, service provided, accessibility of human and fiscal resources, institutional policy, and state nursing regulations.
When considering whether a particular task is within their scope of practice, nurses should ask themselves the following questions:
- Are there are any restrictions from my state board of nursing against nurses performing this task?
- Does the health care organization’s job description, policies and procedures, or credentialing documents prohibit me from performing this task?
- Are there any established organizational or community precedents against nurses performing this task?
- Do I have the requisite knowledge and skills to perform this task correctly and safely?
- Does this task require oversight by a physician (Van Wicklin, 2021).
It is important to remember that tasks within one nurse’s scope of practice may not be within another nurse’s scope of practice. Nurses may only perform those tasks for which they possess the requisite knowledge and skill to perform the task safely and correctly.
The employing facility is responsible for providing education and verifying and documenting the competency of their employees, including nurses functioning in the expanded RNFA role. The AORN Core Curriculum for the RN First Assistant (Seifert, 2014) includes a competency verification tool for the RNFA that facility personnel can use to verify competency of an RNFA.

Sharon Ann Van Wicklin, PhD, RN, CNOR, CRNFA(E), CPSN-R, PLNC, FAAN, ISPAN-F
References
American Association of Critical Care Nurses. (n.d.). https://www.aacn.org/certification?tab=First-Time%20Certification.
American Nurses Association. (n.d.). Scope of practice. https://www.nursingworld.org/practice-policy/scope-of-practice.
AORN. (2018). Position Statement on RN First Assistants. https://www.aorn.org/guidelines/clinical-resources/rn-first-assistant-resources.
AORN. (2013). The RN First Assistant (RNFA) Standards of Practice. https://www.aorn.org/docs/default-source/guidelines-resources/rnfa-standards-of-practice.pdf
Seifert, P. C. (2014). Core curriculum for the RN first assistant (5th ed.). AORN, Inc. https://shop.aorn.org/core-curriculum-for-the-rn-first-assistant-5th-edition-e-book/.
Stuckey, C. H., & Wymer, J. A. (2020). Progressing toward certification as the national standard for nursing. Nursing Forum, 55(3), 531-534.
Van Wicklin, S. A. (2021). Determining scope of practice. Plastic Surgical Nursing, 41(1), 40-42.
info@nascertification.org | 866-681-NASC (6272) | Contact
© Copyright 2020 NASC




Excellent Job..it is mandatory read it for all CRNFA….